Enhancing surgical decision-making: the critical need for structured ultrasound training in residency. A case report of acute necrotic cholecystitis
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
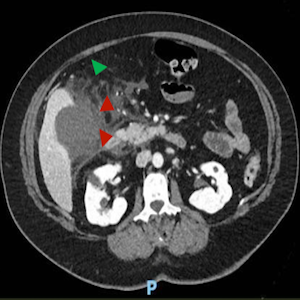
Acute necrotic cholecystitis (ANC), marked by gallbladder wall necrosis, carries high morbidity if diagnosis and treatment are delayed. Ultrasound is the first-line imaging for suspected cholecystitis, but its sensitivity for necrosis is limited. This case underscores the value of surgical ultrasound competency in emergency decision-making. A 57-year-old woman with diabetes, asthma, and hypothyroidism presented with severe epigastric pain and systemic inflammation. Emergency ultrasound showed gallbladder wall thickening, pericholecystic fluid, and gallstones. CT confirmed necrosis with possible microperforation. An informal ultrasound by surgical residents later that day identified microperforations, expediting the decision for subtotal laparoscopic cholecystectomy. Surgery was successful, and recovery was uneventful. Ultrasound, when performed by trained surgical teams, enables rapid diagnosis and management of complex cholecystitis. Structured ultrasound training during residency could enhance diagnostic accuracy, reduce treatment delays, and improve outcomes in acute surgical emergencies.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.







